MODULE 2
PATIENT HISTORY
This module we are focussing on the past tenses and the present perfect. It is very important to make sure you know what to tell your patients when they ask you questions or when you answer questions. We will be working on telephoning skills and skills that you need when working at the desk.
(Deze module focust op de verleden tijd en de voltooid tegenwoordige tijd. Het is erg belangrijk ervoor te zorgen dat je weet wat je tegen patiënten moet zeggen als ze vragen hebben. We gaan werken met telefoongesprekken en andere vaardigheden die je nodig hebt in de praktijk.)
PRACTICE YOUR GRAMMAR!
On the website Nedercom you can practice the grammar topics. If you go to the website and follow the instructions you can choose from a selection of programs. In English class we practice with the programs High Five and Mind the Gap.
The topics for this module are: past simple, past continuous, present perfect.
(Op de website Nedercom kun je oefenen met de grammatica topics. Als je naar de website gaat en de instructies volgt kun je een programma kiezen. In de Engelse lessen werken met de programma's High Five en Mind the Gap.
De grammaticaonderdelen van deze module zijn: past simple, past continuous en present perfect.)

VOCABULARY
FINDING ANSWERS
EXERCISE:
Find answers to the following questions:
- What is tooth decay, and what causes it?
- How does poor dental hygiene contribute to tooth decay?
- What are some common symptoms of tooth decay?
- Describe two methods for preventing tooth decay.
- Why is it important to brush your teeth regularly?
- What role does sugar play in tooth decay?
- How often should you visit the dentist for a check-up?
- Can you name two foods or drinks that are harmful to dental health?
- What are some possible consequences of untreated tooth decay?
- Explain why fluoride is beneficial for dental health.
Discuss with a classmate what you found online or what you already know and compare answers.
LISTENING, WRITING AND SPEAKING
EXERCISE:
Watch the following video. Now you are going to do two exercises. You can decide for yourself whether you want to give an instruction for gingivitis or periodontitis.
OPTION 1: Instructie over Gingivitis voor patiënten
Schriftelijke Opdracht (500 woorden):
In deze schriftelijke opdracht dien je een gedetailleerde instructie te schrijven over gingivitis voor een patiënt. Hier zijn enkele punten die je moet behandelen:
- Introductie: Leg kort uit wat gingivitis is en waarom het belangrijk is om het te behandelen. Verduidelijk dat gingivitis een ontsteking van het tandvlees is die kan leiden tot bloeden, roodheid en zwelling.
- Oorzaken en Risicofactoren: Bespreek de oorzaken van gingivitis, zoals slechte mondhygiëne, tandplakophoping, roken, stress en slechte voeding. Identificeer risicofactoren die het risico op gingivitis kunnen verhogen, zoals diabetes, hormonale veranderingen en bepaalde medicijnen.
- Symptomen: Beschrijf de symptomen van gingivitis, waaronder rood, gezwollen tandvlees, bloeding tijdens het tandenpoetsen, slechte adem en gevoeligheid. Moedig de patiënt aan om deze symptomen serieus te nemen en om zo snel mogelijk een tandarts te raadplegen voor een diagnose en behandeling.
- Preventie: Geef advies over hoe gingivitis te voorkomen, zoals regelmatig tandenpoetsen, flossen en gebruik maken van mondspoeling. Benadruk het belang van regelmatige controles bij de tandarts en mondhygiënist om tandplak en tandsteen te verwijderen en vroege tekenen van gingivitis op te sporen.
- Behandeling: Bespreek mogelijke behandelingsopties voor gingivitis, zoals professionele reiniging, tandsteenverwijdering, mondspoelingen en medicatie. Leg uit dat vroege behandeling van gingivitis kan helpen voorkomen dat het zich ontwikkelt tot ernstigere tandvleesaandoeningen zoals parodontitis.
OPTION 2: Instructie over Parodontitis voor patiënten
Schriftelijke Opdracht (500 woorden):
In deze schriftelijke opdracht dien je een gedetailleerde instructie te schrijven over parodontitis
voor een patiënt. Hier zijn enkele punten die je moet behandelen:
- Introductie: Leg kort uit wat parodontitis is en waarom het belangrijk is om het te behandelen. Verduidelijk dat parodontitis een ernstige tandvleesaandoening is die kan leiden tot verlies van tanden en andere complicaties.
- Oorzaken en Risicofactoren: Bespreek de oorzaken van parodontitis, zoals slechte mondhygiëne, roken, genetische aanleg en andere medische aandoeningen. Identificeer risicofactoren die het risico op parodontitis kunnen verhogen, zoals diabetes, stress en slechte voeding.
- Symptomen: Beschrijf de symptomen van parodontitis, waaronder rood, gezwollen tandvlees, bloeden tijdens het tandenpoetsen, losse tanden en slechte adem. Moedig de patiënt aan om op te letten op deze symptomen en om onmiddellijk een tandarts te raadplegen als ze optreden.
- Preventie: Geef advies over hoe parodontitis te voorkomen, zoals regelmatig tandenpoetsen, flossen en spoelen met mondwater. Benadruk het belang van regelmatige controles bij de tandarts en mondhygiënist om vroege tekenen van parodontitis te detecteren en te behandelen.
- Behandeling: Bespreek mogelijke behandelingsopties voor parodontitis, waaronder professionele reiniging, antibioticatherapie, flapoperaties en tandheelkundige implantaten. Leg uit dat de behandeling kan variëren afhankelijk van de ernst van de parodontitis en individuele factoren.
IMPORTANT INFO
Als je in een tandartspraktijk werkt en Engels moet gebruiken, zijn er een paar cruciale dingen die je moet weten en kunnen:
1. Communicatie met Patiënten:
- Basale conversatie: Je moet in staat zijn om patiënten vriendelijk te begroeten, vragen hoe het met hen gaat en hen gerust te stellen.
- Uitleg van behandelingen: Het is belangrijk dat je behandelingen in eenvoudige termen kunt uitleggen, bijvoorbeeld wat een controle, röntgenfoto, vulling of wortelkanaalbehandeling inhoudt.
- Instructies geven: Je moet in staat zijn om duidelijke mondverzorgingsinstructies te geven, zoals het uitleggen hoe te poetsen, flossen, of instructies na een behandeling.
2. Medische Terminologie:
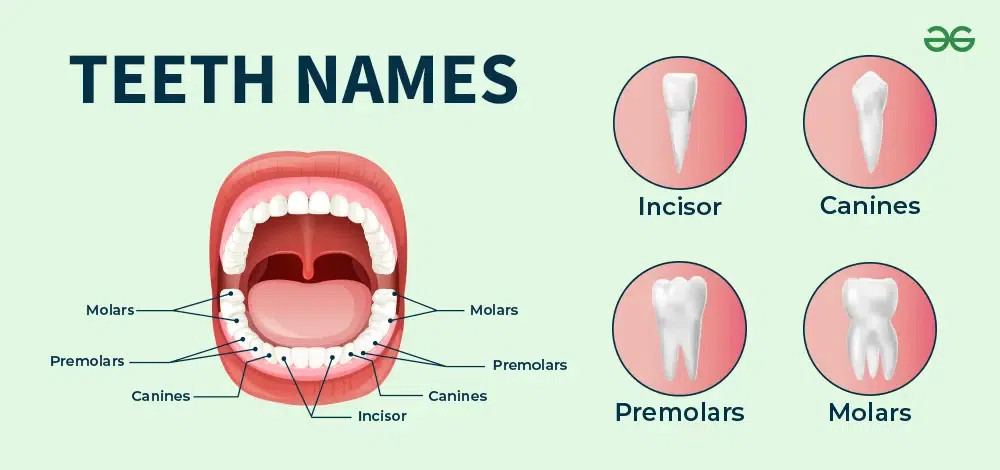
- Tandheelkundige termen: Bekend zijn met veelvoorkomende tandheelkundige termen in het Engels zoals "cavity" (gaatje), "plaque" (plak), "gingivitis" (tandvleesontsteking), en "anesthesia" (verdoving).
- Anatomie van de mond: Basiskennis van de Engelse namen van tanden, tandvlees, en andere delen van de mond is essentieel.
3. Administratie en Afspraakbeheer:
- Afspraak maken: Je moet in staat zijn om afspraken in te plannen en bevestigen, en eventueel wijzigingen of annuleringen door te geven.
- Verzekeringszaken: Basiskennis van tandheelkundige verzekeringen en de terminologie die daarbij hoort kan handig zijn, zoals "coverage" (dekking) en "claim" (claim).
4. Luisteren en Begrip:
- Patiëntvragen: Je moet goed kunnen luisteren naar de vragen of zorgen van patiënten en deze accuraat kunnen beantwoorden.
- Verschillende accenten: Het helpt om vertrouwd te raken met verschillende Engelse accenten, aangezien patiënten van verschillende afkomst kunnen komen.
Deze vaardigheden zorgen ervoor dat je effectief kunt communiceren en een hoge kwaliteit van zorg kunt bieden aan Engelssprekende patiënten.
READING
EXERCISE:
Read the text. Look up words you do not know.
ROOT
CANAL TREATMENT
A root canal is a
dental procedure to fix a tooth that cannot be filled or restored any other
way. If the tooth is severely decayed into the pulp of the tooth and / or
infected, root canal treatment is usually the only option to save the tooth.
Your regular dentist might do the root canal , but he / she may send you to an
endodontist.
What
to Expect
After the dentist numbs your tooth, he / she may use a rubber dam to keep the
tooth area dry and free of saliva. A rubber dam is simply a piece of rubber
that fits over the tooth and isolates it from the rest of the mouth. The
dentist will then prepare the tooth by drilling an opening.
After the dentist removes all of the decay and bacteria, he / she will use root canal files to clean out the canals (roots) of the tooth. Root canal files are small instruments that increase in diameter and fit down into the canals enabling the dentist to remove the pulp of the tooth.
Some dentists like to wait a week or two before they finish a root canal, to make sure that there is no discomfort or further infection. If this is the case, the dentist will thoroughly clean the tooth and usually put some soothing medicine inside and seal it closed with a temporary filling material.
At the final stage of a root canal treatment, the dentist will usually fill the canals with a rubber filling material called gutta percha. After the canals are filled, a regular filling will be placed in the tooth.
Question:
What is a Cavity?
Answer: A cavity is a
hole in the tooth that is caused by decay. Decay occurs when plague, the
sticky substance that forms on teeth, combines with the sugars and / or
starches of the food we eat. This combination produces acids that attack tooth
enamel. The best way to prevent tooth decay is brushing twice a day, flossing
daily and going to your regular dental checkups. Eating healthy foods and
avoiding snacks and drinks that are high in sugar are also ways to prevent
decay.
Afraid
of the dentist
Afraid of the dentist?
Be careful not to avoid the dentist too much because, in my opinion, there is nothing
worse than a toothache. The pain is so intense and nothing seems to make it go
away. I would personally rather be in labour than have a severe toothache. Fortunately,
most toothaches can be prevented by visiting your dentist for regular checkups.
Unfortunately, many people wait until they have a severe toothache before going
to the dentist.
In my dental career, I have noticed that the two major reasons that most people avoid the dentist are finances and dental fears and phobias.
Dental
Fears and Phobias
For a lot of people,
the fear of going to the dentist is so intense that they won't even make an appointment.
The end result of this is usually severe dental problems.
Dental problems do not get better and they do not go away. It usually takes a severe toothache to get this type of person into a dental office and by this time, the tooth that is aching so badly will probably need a root canal and crown to save the tooth.
I am embarrassed to admit this, but I also have a huge fear of the dentist. Lucky for me, I have discovered the secret of limiting my visits to the dentist. I will share the 3 steps of this secret with you:
1. Brush twice a day
2. Floss Daily
3. See your dentist for regular checkups.
When you consider the alternatives, these 3 steps are simple.
Dental
Checkups Could Save Your Life
Dental checkups and
cleaning are a whole lot easier than root canals and crowns and a lot less expensive.
Regular checkups could also save your life by detecting any early signs of oral
cancer.
My cousin's husband died this week of oral cancer. I have another cousin on a different side of the family that is undergoing extensive radiation for oral cancer. Oral cancer is highly curable if it is diagnosed and treated early. Your dentist and hygienist are trained to screen you for oral cancer at your regular checkups.
Bottom
Line
If you don't want to pay a
lot for dental work, follow the three steps above. I can't guarantee that you won't
ever need a root canal or other major work, but the best thing you can do for
your mouth is to take care of it. Don't think of your dentist as an "emergency
room" where you will only go if you have an excruciating toothache.
EXERCISE:
Read the text. Look up words you do not know.
Cosmetic dental Treatment and the orthodontist
And why do people get it done?
What is the difference between an orthodontist and a normal dentist?
What's an Orthodontist?
Just like baseball and gymnastics are types of sports, an orthodontist is a type of dentist. An orthodontist prevents and treats mouth, teeth, and jaw problems. Using braces, retainers, and other devices, an orthodontist helps straighten a person's teeth and correct the way the jaws line up.
Straight teeth and aligned jaws create nice smiles. On top of that, when your jaws and teeth are well aligned, it's easier to chew food. Orthodontic care can even help prevent snoring!
So why would you go to the orthodontist? Your dentist or one of your parents might recommend it because they see a problem with your teeth or jaws. Or a kid who doesn't like the way his or her teeth look might ask to see an orthodontist.
Orthodontists treat kids for many problems, including having crowded or overlapping teeth or having problems with jaw growth and tooth development. These tooth and jaw problems may be caused by tooth decay, losing baby teeth too soon, accidents, or habits like thumb sucking. These problems also can be genetic or inherited, meaning that they run in a person's family.
When Should a Kid Go to the Orthodontist?
There's no set age for a kid to visit the orthodontist — some kids go when they're 6, some kids go when they're 10, and some go while they're teens. Even adults visit the orthodontist for treatment. Many orthodontists say a kid should see an orthodontist before age 7 so any problems can be spotted early. That doesn't mean a kid will get braces right away. But the orthodontist will know which problems exist and can choose the best time to start treatment.
What Happens at the Orthodontist?
When you make your first trip to the orthodontist, you'll visit an office that looks a lot like your dentist's office. You'll sit in a dentist chair and the orthodontic technician or assistant might take X-rays or computer pictures of your mouth and teeth. The X-rays and pictures show the orthodontist where the teeth are positioned and whether you have teeth that haven't come in yet.
The technician also may make a mold (or impression) of your teeth by pressing a tray of gooey material into your top and bottom teeth. When the mold is removed, there will be a perfect impression of the shape and size of your teeth. A mold helps the orthodontist decide how to straighten your teeth.
The orthodontist will examine your teeth, mouth, and jaws. He or she may ask you to open wide or bite your teeth together. He or she may ask questions about whether you have problems chewing or swallowing or whether your jaws ever click or pop when you open your mouth. The orthodontist may tell you and your parent that your teeth and jaws are fine. Or he or she might recommend that you get braces or a retainer.
EXERCISE:
Read the text. Look up words you do not know.
Cavities and tooth decay
Cavities are areas in the hard surface of your teeth that are damaged. These areas of tooth decay become tiny openings or holes that can lead to a serious toothache, infection and tooth loss. There are several causes of cavities, including bacteria in your mouth, snacking a lot, sipping sugary drinks and not cleaning your teeth well.
Cavities and tooth decay are among the world's most common health problems. They're especially common in children, teenagers and older adults. But anyone who has teeth can get cavities, including babies.
If cavities aren't treated, they get larger and affect deeper layers of your teeth. Regular dental visits and good brushing and flossing habits are the best ways to protect your teeth from cavities.
Symptoms
The symptoms of cavities vary, depending
on how many you have and where they're located. When a cavity is just
beginning, you may not have any symptoms. As the decay gets larger, it may
cause symptoms such as:
- Toothache and other pain.
- Tooth sensitivity.
- Mild to sharp pain when eating or drinking something sweet, hot or cold.
- Holes or pits in your teeth that you can see.
- Brown, black or white staining on any surface of a tooth.
- Pain when you bite down.
When to see a dentist
You may not be
aware that a cavity is forming. That's why it's important to have regular
dental checkups and cleanings, even when your mouth feels fine. But if you have
a toothache or mouth pain, see your dentist as soon as possible.
Causes
Tooth decay causes cavities. This is a process that occurs over time.
Here's how tooth decay
happens:
- Plaque forms. Dental plaque is a clear sticky film that coats your teeth. It's due to eating a lot of sugars and starches and not cleaning your teeth well. When you don't clean sugars and starches off your teeth, bacteria quickly begin feeding on them and forming plaque. Plaque that stays on your teeth can harden under or above your gumline into tartar. Tartar makes plaque harder to remove and creates a shield for bacteria. A dental professional needs to remove this plaque.
- Plaque attacks. The acids from bacteria remove minerals in your tooth's hard, outer enamel. This erosion causes tiny openings or holes in the enamel — the first stage of cavities. Once areas of enamel are worn away, the bacteria and acid can reach the next layer of your teeth, called dentin. This layer is softer than enamel and less resistant to acid, causing your teeth to be more sensitive.
- Damage continues. As tooth decay happens, the bacteria and acid move through your teeth to the inner tooth material (pulp) that contains nerves and blood vessels. The pulp becomes swollen and irritated from the bacteria. Because there is no place for the swelling to expand inside of a tooth, the nerve becomes pressed, causing pain. Sometimes pain and damage can spread outside of the tooth root to the bone, causing bone loss around the tooth and even reaching nearby teeth.
Risk factors
Anyone who has teeth can get cavities, but these factors raise the risk:
- Tooth location. Decay most often occurs in your back teeth — your molars and premolars. These teeth have lots of grooves, pits and crannies, and multiple roots that can collect food particles. That's why they're harder to keep clean than your smoother, easy-to-reach front teeth.
- Certain foods and drinks. Foods that cling to your teeth for a long time are more likely to cause decay than foods that are easily washed away by saliva. These foods include milk, ice cream, honey, sugar, soda, dried fruit, cake, cookies, hard candy and mints, dry cereal, and chips.
- Snacking or sipping a lot. When you snack or sip sugary drinks a lot, you give mouth bacteria more fuel to make acids that attack your teeth and wear them down. And sipping soda or other acidic drinks throughout the day helps create a continual acid bath over your teeth.
- Bedtime baby feeding. When babies are given bedtime bottles filled with milk, formula, juice or other liquids that have sugar, these beverages remain on their teeth for hours while they sleep. This feeds bacteria that can cause decay. This damage often is called baby bottle tooth decay. Similar damage can occur when toddlers wander around drinking from a sippy cup filled with these beverages.
- Not brushing your teeth well. If you don't clean your teeth soon after eating and drinking, plaque forms quickly, and the first stages of decay and gingivitis can begin.
- Not getting enough fluoride. Fluoride, a naturally occurring mineral, helps prevent cavities. It also can reverse the earliest stages of tooth damage. Because of its benefits for teeth, fluoride is added to many public water supplies. It's also a common ingredient in toothpaste and mouth rinses. But bottled water usually does not contain fluoride.
- Younger or older age. In the U.S., cavities are common in very young children and teenagers. Older adults also are at higher risk. Over time, teeth can wear down and gums may recede, making teeth more likely to decay. Older adults also may use more medicines that reduce saliva flow, raising the risk of tooth decay.
- Dry mouth. Dry mouth is caused by a lack of saliva. Saliva helps prevent tooth decay by washing away food and plaque from your teeth. Substances found in saliva also help counter the acid produced by bacteria. Certain medicines, some medical conditions, radiation to your head or neck, or certain chemotherapy drugs can raise your risk of cavities by reducing saliva production.
- Worn fillings or dental devices. Over the years, dental fillings can weaken, begin to break down or get rough edges. This allows plaque to build up more easily and makes it harder to remove. Dental devices can stop fitting well, allowing decay to begin under them.
- Heartburn. Heartburn, a common symptom of gastroesophageal reflux disease (GERD), can cause stomach acid to flow into your mouth. This is called reflux. It can wear away the enamel of your teeth and cause a lot of damage. This exposes more of the dentin to bacteria, creating tooth decay. Your dentist may recommend that you talk with your healthcare professional to see if GERD is causing your enamel loss.
- Eating disorders. Anorexia and bulimia can lead to a lot of tooth erosion and cavities. Stomach acid from repeated vomiting, called purging, washes over the teeth and begins eating away at the enamel. Eating disorders also can get in the way of saliva production.
Complications
Cavities and tooth decay are so common that you may not take them seriously.
And you may think that it doesn't matter if children get cavities in their baby
teeth. But cavities and tooth decay can have serious and lasting complications,
even for children who don't have their permanent teeth yet.
Complications of cavities may
include:
- Pain.
- Abscess — a bacterial infection that causes a pocket of pus to form in a tooth.
- Swelling or pus around a tooth.
- Damage or broken teeth.
- Chewing problems.
- Positioning shifts of teeth after tooth loss.
When cavities and decay become serious, you may have:
- Pain that makes it hard to live your daily life.
- Weight loss or nutrition problems because it's painful or difficult to eat or chew.
- Tooth loss, which may affect your appearance, confidence and self-esteem.
- In rare cases, a tooth abscess, which can lead to more-serious or even life-threatening infections.
Prevention
Good oral and dental hygiene can help keep you from getting cavities. Here are
some tips to help prevent cavities. Ask your dentist which tips are best for
you.
- Brush with fluoride toothpaste after eating or drinking. Brush your teeth at least twice a day, and ideally after every meal, using toothpaste with fluoride. To clean between your teeth, floss or use an interdental cleaner. This cleaner helps reach areas where a toothbrush can't reach.
- Rinse your mouth. If your dentist feels that you have a high risk of getting cavities, a mouth rinse with fluoride may be recommended.
- Visit your dentist regularly. Get professional teeth cleanings and regular oral exams, which can help prevent problems or spot them early. Your dentist can recommend a schedule that's best for you.
- Consider dental sealants. A sealant is a protective plastic coating applied to the chewing surface of back teeth. It seals off grooves and crannies that tend to collect food, protecting tooth enamel from plaque and acid. The Centers for Disease Control and Prevention recommends sealants for all school-age children. Sealants may last for several years before they need to be replaced, but they need to be checked regularly.
- Drink some tap water. Most public water supplies have added fluoride, which can reduce tooth decay greatly. If you drink only bottled water that doesn't contain fluoride, you'll miss out on the benefits of fluoride.
- Avoid snacking and sipping a lot. Whenever you eat or drink beverages other than water, you help your mouth bacteria create acids that can destroy tooth enamel. If you snack or drink throughout the day, your teeth are under constant attack.
- Eat tooth-healthy foods. Some foods and beverages are better for your teeth than others. Avoid foods that get stuck in grooves and pits of your teeth for long periods, or brush soon after eating them. Foods such as fresh fruits and vegetables increase saliva flow, and unsweetened coffee, tea and sugar-free gum help wash away food particles.
- Consider fluoride treatments. Your dentist may recommend periodic fluoride treatments, especially if you aren't getting enough fluoride through fluoridated drinking water and other sources. Your dentist also may recommend custom trays that fit over your teeth to apply prescription fluoride if your risk of tooth decay is very high.
- Ask about antiseptic and disinfecting treatments. If tooth decay is likely — for example, because of a medical condition — your dentist may recommend special antiseptic and disinfecting mouth rinses like chlorhexidine or other treatments to cut down on harmful bacteria in your mouth. Unless your dentist tells you otherwise, mouth rinses, also called mouthwash, generally are not recommended for children younger than the age of 6 so they don't swallow too much of it.
- Combined treatments. Chewing sugar-free gum along with prescription fluoride and an antibacterial rinse can help reduce the risk of cavities. But in some people, xylitol, which is often found in sugar-free gum or sugar-free candies, may cause gas or diarrhoea if consumed in large amounts.
SOURCE: www.mayoclinic.org/diseases-conditions/cavities/symptoms-causes/syc-20352892
LISTENING
- Watch the provided video attentively.
- Listen carefully to the dialogue and instructions throughout the video.
- We will then discuss in class.